InetSoft Webinar: Faster Better Cheaper Analytics and Decision-Making
Below is the continuation ofthe transcript of a Webinar hosted by InetSoft on the topic of Machine Learning and Healthcare Analytics. The presenter is Abhishek Gupta, Product Manager at InetSoft, and the guest is Jim Reynolds, CTO at Health Analytica.
Abhishek: Okay well, faster, better, cheaper analytics and decision-making, these are the goals I see very often in many verticals. The stakes here and the scale here just seem to be much larger. So speaking of scale you have a fourth generation analytic solution. Tell us at the high level a little bit about that before we delve a bit more detail about the technological requirements. What is it that you've developed that helps deal with these issues of scale?
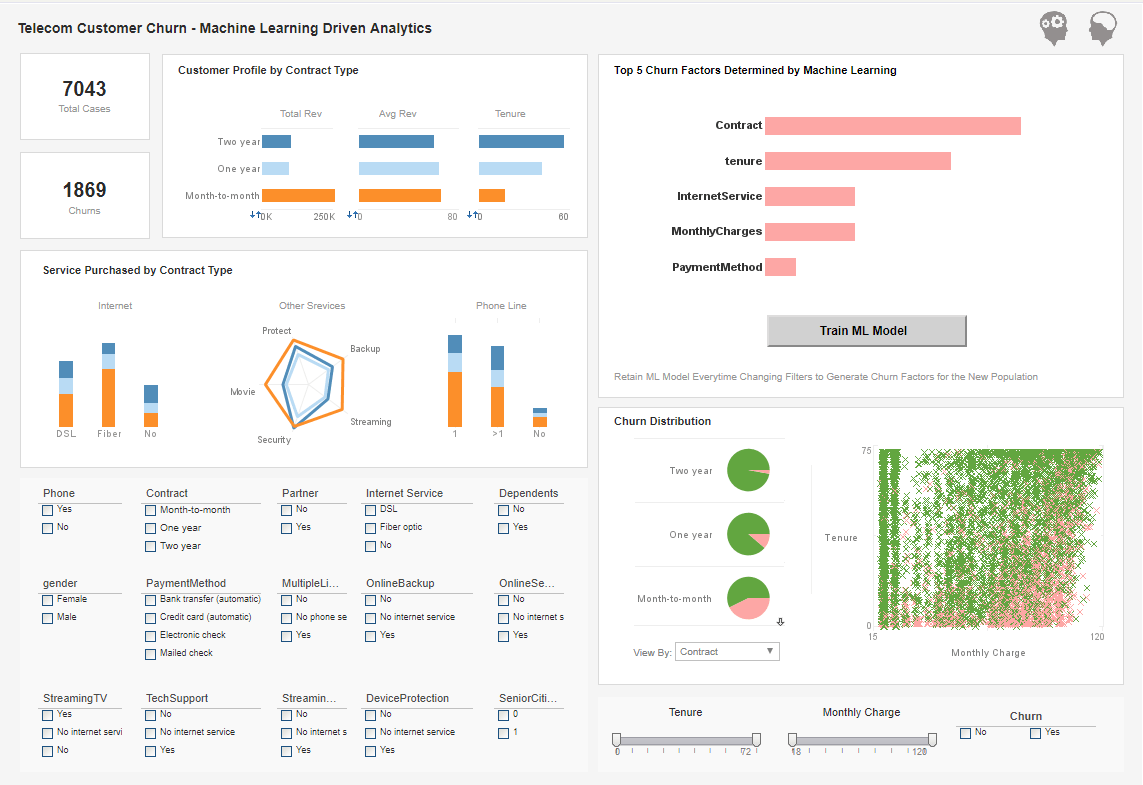
Jim: So our platform really harnesses big data pipeline technology that makes it accessible to users in a very interactive and highly seamless in immersive environment will allows them to zero in on pieces of data. And the analytic tools allow them to make decisions very quickly and with very high quality confidence that the data is going to really help to make a high quality decision.
So we bring large amounts of claims and other sources of data together, and we fuse that together into a very large data set, and we run a lot of machine learning analytics over the top of that and provide a variety of visualizations and navigational constructs for them.
We allow them to see what the provider looks like in terms of how much money that they've been billing, what kinds of activities have they been doing, what relationships they have to other providers or other institutions and to really surface in a very visual way that interconnectivity that they had into a healthcare network or a plan.
| #1 Ranking: Read how InetSoft was rated #1 for user adoption in G2's user survey-based index | Read More |
In addition to that we allow investigators to zero in on patterns of bad behavior, and in a very quick and seamless way identify the exact services that should not have been occurring and then contextually apply dollar values or a quantities or areas, geographic areas that allow people to understand this event shouldn't be happening.
Then they can assess how significant that it is and appropriately allocate resources. If the same thing is happening once or twice, it's not that much of an issue to go invest big resources in, but if you're spending tens or hundreds of millions of dollars in an area, and you want to zero in on the bad parts of that big spend, you need tools that really help you get to the bottom of that and our machine learning analytic solution has got full big data spread with really good user interfaces that allows you to achieve those goals.
Abhishek: Okay, I'd just like to offer a friendly reminder to our audience, add your questions to the online interface where indicated. Jim and I will be happy to fill those towards the end of our presentation. Okay, Jim it sounds like you're biting off an awful lot to chew with this approach with these solutions, tell me a little bit about the data challenges.
One other thing we hear is yeah we've got certainly a lot to accomplish with our platform, but we can't do it until we get the data in a place and in a fashion that we can then analyze. So tell us a little bit about the data challenges. What hampers your clients as they seek to prevent fraud and gather and use the data to do that.
Jim: Well a lot of our clients have a variety of sources of data, and they are more rich and complicated and in reality messy. Healthcare claims just come in so many different shapes and sizes and quality and in order to get that data cleaned up and processed and then captured in a way that unifies it across the board that it can be analyzed, that's the first challenge with any big data project.
 |
View live interactive examples in InetSoft's dashboard and visualization gallery. |
In the case of healthcare we have to do not just cleaning up the data, but we've also got to go in and really instrument it with things like where you would typically see in a master data management environment which is we have to be able to identify a provider, and we have to do it in a way that a provider is recognizable across all the different programs that they participate in.
So that's something else that we offer as part of our data curation platform. We have to be able to manage the identities of all the participants in the healthcare system. Then we fuse data from other sources. We'll take things from government open data sources, and we will fuse this into the environment to really enrich it to make it much more understandable.
Healthcare is full of acronyms and codes, and even a simple act of making reference data easily accessible to people is really challenging, and people spend a lot of time looking up simple things like codes. Making that all immersively available is part of what we do at the very early stages of our data curation process.
| Previous: Healthcare Analytics and Data Science |